Pharyngeal Sense Electrical Stimulation for Treatment of Dysphagia
Pharyngeal Sense electrical stimulation (PSES) is a therapeutic intervention used to treat dysphagia, particularly in patients with neurological conditions such as stroke. Dysphagia, or difficulty swallowing, can result in severe complications like aspiration pneumonia, malnutrition, and dehydration.
Key Aspects of Pharyngeal Sense Electrical Stimulation (PSES):
1. Mechanism of Action:
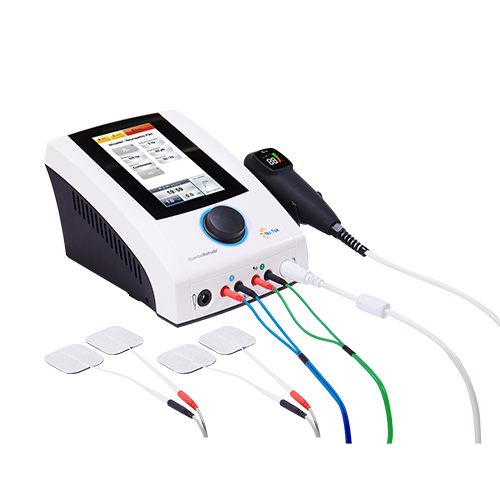
- PSES involves the use of electrical impulses to stimulate the pharyngeal muscles, which are responsible for swallowing. Electrodes are typically placed through the nose or mouth to stimulate the nerves controlling these muscles.
- The electrical impulses trigger a response that enhances neuromuscular coordination and strength in the swallowing mechanism, often through cortical reorganization or adaptation in the brainstem.
2. Procedure:
- A catheter with electrodes is inserted transnasally or orally into the pharyngeal region.
- Electrical stimulation is delivered at specific frequencies and intensities, typically lasting 10-15 minutes per session.
- The procedure is usually performed in a clinical setting by trained professionals and may be repeated over multiple sessions.
3. Indications:
- PSES is primarily indicated for dysphagia resulting from neurological damage, such as after a stroke, traumatic brain injury, or neurodegenerative diseases.
- It can also be used in patients with prolonged dysphagia in intensive care or post-surgery recovery.
4. Clinical Evidence:
- Studies have shown PSES can improve swallowing function by enhancing the sensory feedback loop involved in the swallowing reflex, leading to better control of the pharyngeal muscles.
- Some research suggests improvements in swallowing efficiency, reduced aspiration risk, and shorter recovery times in stroke patients treated with PSES.
5. Safety and Side Effects:
- PSES is generally well-tolerated, though minor side effects may include discomfort or a gag reflex during the procedure.
- Long-term side effects are rare, but ongoing monitoring is essential to ensure correct electrode placement and stimulation parameters.
6. Comparison with Other Treatments:
- PSES is often combined with traditional swallowing therapy, such as muscle exercises and dietary modifications.
- It may offer an alternative to more invasive procedures like feeding tubes or surgeries in severe cases of dysphagia.
7. Future Applications:
- Research is ongoing to expand the application of PSES beyond neurological dysphagia, potentially offering benefits for patients with mechanical swallowing issues or age-related dysphagia.
In conclusion, Pharyngeal Sense Electrical Stimulation offers a promising, non-invasive therapy for dysphagia, particularly in patients with neurological damage. By improving swallowing coordination and function, PSES helps reduce the risks associated with dysphagia, enhancing quality of life for affected individuals.


 中文
中文 Español
Español Français
Français Português
Português