Sports Medicine
Sports medicine is a multidisciplinary field that integrates various specialties to optimize health, performance, and injury management for athletes and physically active individuals. Its system is broad and covers several key areas:
1. Injury Prevention
Biomechanics: Understanding how the body moves and identifying movement patterns that could lead to injury.
Strength and Conditioning: Programs that help athletes build strength, endurance, and flexibility to prevent injuries.
Nutrition: Guidance on proper diet and hydration strategies to fuel performance and aid in recovery.
Equipment and Technique: Ensuring proper use of sports equipment and teaching proper techniques to reduce injury risk.
2. Injury Diagnosis
Musculoskeletal Injuries: Sports medicine professionals diagnose acute injuries such as sprains, fractures, and dislocations, as well as overuse injuries like tendinitis and stress fractures.
Imaging: Diagnostic tools like X-rays, MRIs, CT scans, and ultrasound are used to assess injuries and their severity.
Functional Assessment: Evaluating how injuries affect movement, strength, and performance.
3. Treatment of Injuries
Non-surgical Interventions: This can include rest, physical therapy, bracing, and medications for pain and inflammation (like NSAIDs).
Surgical Interventions: In severe cases, surgical procedures may be necessary to repair torn ligaments (e.g., ACL), fractures, or dislocations.
Regenerative Medicine: Some sports medicine practices involve cutting-edge treatments like platelet-rich plasma (PRP) therapy or stem cell treatments to accelerate healing.
4. Rehabilitation and Recovery
Physiotherapy: Tailored programs to help athletes recover strength, mobility, and function after an injury. Physiotherapy may involve:
Manual therapy (joint mobilizations, massage)
Exercise therapy (strengthening, flexibility, proprioception)
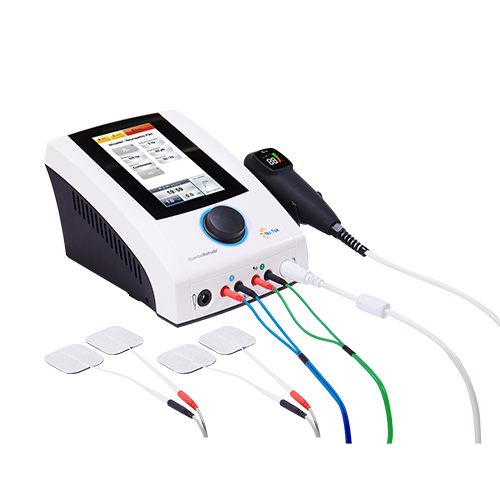
Modalities (ultrasound, electrotherapy, cryotherapy)
Return-to-Play Protocols: These are step-by-step guidelines to help athletes safely return to their sport after an injury. It often involves a gradual increase in intensity and volume of training.
5. Performance Enhancement
Strength and Conditioning Coaching: Programs designed to improve specific aspects of performance, such as strength, speed, agility, and endurance.
Mental Health and Sports Psychology: Addressing the mental aspects of sports, including focus, anxiety, motivation, and goal setting.
Nutrition and Supplementation: Tailored nutritional plans to optimize energy levels, muscle recovery, and overall performance.
6. Special Populations and Conditions
Adolescent Athletes: Addressing unique issues related to growth and development, including the risks of overtraining.
Female Athletes: Considerations related to the menstrual cycle, hormonal influences on performance, and higher risks of certain injuries (like ACL tears).
Aging Athletes: Managing the unique needs of older individuals who want to stay active, including the prevention and management of age-related conditions like osteoarthritis.
7. Sports-Related Medical Conditions
Concussions: Diagnosis, management, and rehabilitation protocols for concussions, a common injury in contact sports.
Cardiovascular Health: Addressing heart-related issues in athletes, such as screening for conditions like hypertrophic cardiomyopathy or sudden cardiac arrest risk.
Environmental Concerns: Management of heat-related illnesses, dehydration, altitude sickness, and other environmental factors that can affect performance and safety.
8. Research and Technology in Sports Medicine
Wearable Technology: Devices that track biometric data (heart rate, oxygen levels, movement patterns) to monitor performance and recovery.
Data Analysis: Using statistical and technological tools to analyze player performance, injury risks, and recovery processes.
Emerging Therapies: Advancements in sports medicine, such as shockwave therapy, laser therapy, and tecar therapy, are expanding the options for injury treatment and rehabilitation.
9. Education and Athlete Health Promotion
Athlete Education: Teaching athletes about the importance of training techniques, injury prevention, nutrition, and mental health.
Public Health Initiatives: Encouraging a healthy lifestyle, not only for elite athletes but also for general populations engaged in physical activities.
Multidisciplinary Team in Sports Medicine:
Sports Physicians: Doctors specializing in musculoskeletal issues and overall health in athletes.
Orthopedic Surgeons: Surgeons who perform operations to repair injuries to bones, ligaments, and tendons.
Physical Therapists/Physiotherapists: Experts in rehabilitation and recovery.
Athletic Trainers: Professionals who work directly with athletes to prevent and manage injuries.
Nutritionists/Dietitians: Experts in sports nutrition and dietary plans for performance.
Sports Psychologists: Experts in mental health and the psychological demands of sports.
Exercise Physiologists: Professionals who study how the body responds to physical activity.
This multidisciplinary and comprehensive approach ensures that athletes get the care they need to maximize their performance while minimizing the risk of injury and promoting long-term health.


 中文
中文 Español
Español Français
Français Português
Português